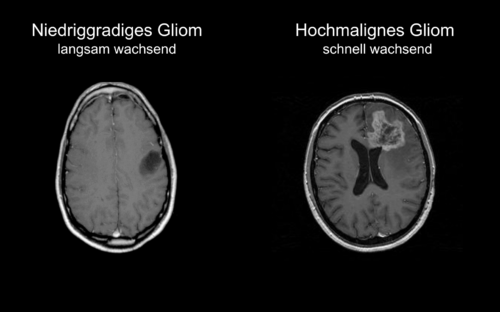
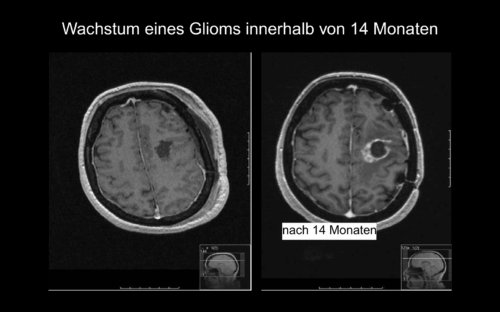
A glioma often grows insidiously – the symptoms arise from pressure on the surrounding brain tissue or through direct influence on brain functions. However, the symptoms of gliomas are diverse and depend heavily on growth, location, and size.
Typical signs include, among others:
- Headaches – often new, pressing, and more strongly felt in the morning
- Epileptic seizures
- Neurological deficits: Vision problems, speech problems, paralysis symptoms
- Personality changes: Irritability, aggressiveness, lack of drive, disorientation, anxieties
- Cognitive disorders: Concentration or memory problems
- Other symptoms: Dizziness, fatigue, insomnia, balance problems, coordination disorders.
Not all affected individuals with a glioma show all symptoms – however, it is important: In case of suddenly occurring or worsening complaints, a neuro-oncological clarification should always be performed.
Gliomas arise from the uncontrolled growth of glial cells. However, the exact cause of a glioma is not yet fully clarified, so it usually remains unknown. Most gliomas occur spontaneously, without a recognizable trigger. In a few affected individuals, a genetic predisposition is present (e.g., Neurofibromatosis Type 1). Gliomas are in the vast majority of cases not hereditary and not caused by stress, diet, or lifestyle.
Modern research shows: Molecular changes that influence growth and therapy response are crucial. Important factors:
- IDH1/2 mutation: Affects the metabolism of tumor cells; often better prognosis.
- 1p/19q codeletion: Typical for oligodendrogliomas; often better therapy response.
- TERT or EGFR changes: Often in aggressive glioblastomas.
- MGMT methylation: Can make chemotherapy more effective.
The exact diagnosis is the key to successful glioma treatment. At the Center for Neuro-Oncological Neurosurgery at Beta Klinik Bonn, we analyze not only the imaging but also your symptoms, your medical history, and possible molecular features – always with a view to the best possible therapy approach.
Our team uses state-of-the-art procedures like functional MRI (fMRI), CT perfusion, contrast-enhanced MRI (cMRI), and if needed, FET-PET. This way, we recognize not only where the tumor is located but also which brain functions might be affected – crucial, for example, for planning an operation. Additionally, we rely on special procedures like 5-ALA fluorescence for surgical planning to make even the finest tumor cells visible and protect healthy tissue wherever possible.
Genetic Tests for Gliomas
Genetic tests should be performed when a glioma is present. They help in planning therapy and treatment.
- To better assess tumor behavior (growth, therapy response).
- To individually adapt therapies (e.g., IDH-mutated tumors often have a better prognosis).
- To avoid unnecessary treatments if the tumor is less aggressive.
Feel free to upload all your findings and documents in our online portal, and we will arrange an appointment with you.
The treatment of a glioma requires a therapy concept based not only on medical standards but on the individual properties of the tumor and the needs of the affected person. At Beta Klinik Bonn, we combine scientifically based procedures with high surgical experience and care. Our goal is to remove as much tumor tissue as possible – without endangering neurological functions – and to control further tumor growth targetedly. We consider WHO grade, tumor location, molecular markers (e.g., IDH, 1p/19q, MGMT), and the personal life situation.
We also stand by families with special care and much experience for gliomas in childhood or adolescence – with gentle diagnostic procedures, individually tailored therapy, and close interdisciplinary care adapted to the special needs of young patients.
The therapy of gliomas typically includes a combination of:
- Neurosurgical resection
- Radiation therapy (radiotherapy)
- Medicinal therapy (chemotherapy, targeted treatments)
The exact treatment depends on the WHO grade, molecular markers (e.g., IDH mutation, 1p/19q codeletion), and tumor location.
The operation of a glioma in the head (surgical resection) is usually the first therapy step. The goal is to remove as much tumor tissue as possible without damaging healthy brain areas. Not every glioma requires an awake surgery. Whether this procedure is applied depends significantly on where the tumor or glioma is located in the brain – particularly if the glioma is near or within function-critical areas.
At Beta Klinik Bonn, we use awake surgeries targetedly when the tumor’s location poses a risk of impairing speech, movement, or other central abilities. Using functional imaging (fMRI), 5-ALA fluorescence (“tumor staining”), and intraoperative tests, we check beforehand whether an operation in the awake state is necessary and safely feasible. The goal is to remove the tumor as far as possible without endangering vital functions. With over 1,000 successfully performed awake surgeries, our team is among the most experienced neuro-oncologists in Germany.
Radiation Therapy
Depending on the WHO grade, the molecular profile of the tumor, and the individual health status, radiation and/or chemotherapy often follows after the operation. For higher-grade gliomas (Grade 3 or progressive Grade 2), the combination of both procedures is often part of the treatment plan.
Radiation therapy aims to destroy remaining tumor cells in the operation area. Planning is done in close coordination with our specialists. The treatment typically occurs over several weeks in small individual doses (fractionated radiotherapy).
Additionally, we advise you on targeted therapies and check whether study participation or new therapy concepts could be sensible in your case.
Chemotherapy
The effectiveness of chemotherapy depends on molecular factors, particularly the MGMT promoter methylation status, which predicts sensitivity to alkylating substances like TMZ. The following options exist:
- Temozolomid (TMZ): Standard for glioblastomas (WHO Grade 4) and some astrocytomas.
- PCV Therapy (Procarbazine, CCNU, Vincristine): Used especially for oligodendrogliomas (with 1p/19q codeletion).
- CeTeG Protocol (CCNU/TMZ combination): An alternative for MGMT-methylated glioblastoma patients, which showed improved overall survival compared to TMZ therapy alone in clinical studies.
Tumor Treating Fields (TTFields)
TTFields are an innovative treatment method that uses low-frequency alternating fields to disrupt tumor cell division. Today, they are part of first-line therapy for glioblastomas, often in combination with chemotherapy to prolong survival.
This non-invasive method requires wearing a special device (Optune®) that continuously generates electric fields. Studies show that TTFields can preserve quality of life and improve progression-free survival.
Accompanying Treatment
For comprehensive treatment and to alleviate the symptoms of gliomas in the head, radiation therapy is supplemented by the following accompanying measures:
- Corticosteroids (Dexamethasone): Short-term use to reduce brain edema.
- Antiepileptics: For seizure prophylaxis.
- Physio-/Occupational therapy & psychooncological care: To improve quality of life.
In addition to medical therapy, we also accompany you psychosocially – through psychooncology, rehab planning, speech therapy, or specialized neurologists in-house. A glioma affects not only the brain – but the whole person. Besides the physical burden, emotional challenges, uncertainties in everyday life, or changes in behavior often arise, which can also heavily burden relatives.
- Our psychooncologist Prof. Dr. med. Marion Rapp supports you and your family in dealing with fears, mood swings, or personality changes.
- We take care of organizing targeted rehab measures – for example, for speech, movement, or concentration disorders.
- Specialized staff for neurology are available to you in-house. We also gladly involve specialized speech therapists and occupational therapists.
- In our neuro-oncological tumor board, experts from neurosurgery, neurology, radiation oncology, and pathology discuss each case individually to determine the best therapy strategy.