Brain Tumor Surgery at Beta Clinic Bonn
Excellence Through Interdisciplinary Collaboration: Our Cooperation with Neuroradiology at Beta Klinik Bonn
At Beta Klinik Bonn, we rely on the power of synergy. In close cooperation with our highly specialized neuroradiologists, we offer precise and innovative diagnostics for brain tumors. Our neuroradiology experts have access to the most modern imaging procedures and specialize in differentiating between true tumor recurrences and treatment-related changes.
Together, we employ an escalating 3-stage diagnostic program – from contrast-enhanced MRI to metabolic imaging via FET-PET and fluorescence-guided biopsy. This interdisciplinary collaboration allows us to make the right decisions for your treatment early and reliably.
Trust our expertise – because a precise diagnosis is the first and most important step towards your individualized therapy.
Your Inquiry
Do you have questions or are you interested in treatment?
You can reach us via our main line at +49 (0)228 90 90 75 0
Brain Tumor Surgery: Your Specialists in Awake Surgery
Brain tumor surgery might sound very frightening at first, especially if you hear that you should be partially awake during the procedure. However, surgery is a crucial step for many affected individuals after a brain tumor diagnosis: an active way to treat the tumor targetedly and improve life expectancy. The operation of brain tumors can help to remove tumorous tissue completely or partially, thereby stopping or significantly slowing tumor growth. This applies to gliomas, glioblastomas, and brain metastases as well as to tumor recurrences of metastases or gliomas.
At the Center for Neuro-Oncological Neurosurgery at Beta Klinik Bonn, our special focus is on function-preserving, high-precision procedures. With over 3,500 successfully performed brain tumor operations, including more than 1,000 specialized awake surgeries, Prof. Dr. med. Michael Sabel and Prof. Dr. med. Marion Rapp are among the most experienced and best neuro-oncological neurosurgeons in Germany – with a clear goal: to preserve your quality of life and neurological function as best as possible.
In collaboration with leading linguists – including Prof. Yosef Grodzinsky (e.g., The Edmond and Lily Safra Center for Brain Sciences & Forschungszentrum Jülich) – we have also developed new methods for preserving speech ability, which are applied exclusively in our center.
Center for Brain Tumors at Beta Klinik Bonn
Your Specialist Team for Complex Brain Tumor Surgery – Experience That Makes the Difference
Are you looking for specialists for brain tumor surgery where more counts than just removing a tumor?
At Beta Klinik, we combine years of neurosurgical experience with methods like awake craniotomy to targetedly protect vital functions.
Table of contents
Awake Surgery for Brain Tumor: Proven Technique for Maximum Safety
For certain brain tumors in sensitive brain regions – particularly near speech, motor, or visual centers – awake surgery (awake craniotomy) is an established surgical procedure. At the Center for Neuro-Oncological Neurosurgery at Beta Klinik Bonn, it is one of our core competencies: More than 1,000 of these highly specialized procedures have already been successfully performed by Prof. Dr. Sabel and Prof. Dr. Rapp. As one of the few clinics in Europe, we also work with laser therapy for treating brain tumors (LITT/Visualase) at Beta Klinik.
What may sound unusual at first is an extremely precise and almost completely pain-free procedure in experienced hands. The goal is to protect the brain as best as possible during surgery – especially where important functions need to be preserved.

“Performing awake surgeries is one of our core competencies. In total, we have already performed over 1,000 awake surgeries and are thus among the most experienced surgeons applying this technique. Awake surgery might sound unusual, but it is a proven procedure to protect your brain. We will accompany you very closely – feel free to ask anything important to you beforehand. Your health is the focus: with this method, we can act targetedly to preserve your quality of life.”
– Prof Dr. med. Marion Rapp
Trust one of Germany’s most experienced teams for brain tumor awake surgeries.
We accompany you empathetically and on equal footing – from preparation to the safe removal of the tumor.
Why is Awake Surgery Performed?
“Some brain tumors lie close to areas responsible for important abilities like speaking, moving, or seeing. Some of these abilities, particularly speech, can only be tested while awake. To protect these important functions, we temporarily anesthetize the tissue around the tumor using electrical impulses. This allows us to determine exactly whether the affected area can be safely removed – or whether it must be preserved to, for example, save your speech. This awake surgery allows us to remove tumor tissue with maximum safety without injuring healthy, function-bearing areas. And most importantly: you will feel no pain – at most a slight feeling of pressure.”
– Prof Dr. med. Michael Sabel
Process of Awake Surgery: Explained Step-by-Step
We discuss the goals of the brain tumor surgery, possible risks, and your individual questions with you in peace. You are, in a way, part of the treatment team. Our team has developed very advanced tests that check your speech and motor functions better than conventionally used tests. These tests are individually adapted and practiced before the brain tumor operation.
At the beginning of the operation, you receive general anesthesia. The scalp is locally anesthetized so that you will feel no pain later during the awake phase. In this phase, access is prepared: we gently open the skull bone, open the dura mater, and perform preparatory tests.
Once we complete this preparation, we gently wake you. Now we specifically test your brain functions by performing the prepared tests. We test speech, movement, or other functions – for example through picture naming or movement tasks – while certain brain areas are electrically stimulated. This way we recognize which areas must be spared. You will feel no pain in this phase – at most a slight feeling of pressure.
After removal of the tumor, anesthesia is continued. The surgical area is closed, and you are monitored and taken to our special ward.
What Happens After Awake Brain Surgery?
After the brain tumor operation, you will be carefully cared for. You will spend the first few days as an inpatient in your room. If you wish, you may already receive visitors. Tailored to your individual situation, further treatment begins quickly – e.g., with radiation therapy or chemotherapy – as well as your individual rehabilitation:
- Possible side effects like headaches or fatigue usually subside after a few days.
- Due to the proximity of the tissue removal to motor, speech, or sensory areas, temporary disturbances of these functions can occur. However, the tissue recovers quickly.
- Speech therapy helps with speech or swallowing disorders.
- Physiotherapy helps with movement problems or hemiplegia.
- Neurocognitive training promotes attention and memory.
- Psychooncological support and coaching offer emotional support.
Very rarely, despite all precautions, permanent damage occurs. It is very important that you understand this and consciously accept this risk. We explain to you very precisely why we want to subject you to this “residual risk.”
Innovative Methods at Beta Klinik: Fluorescence-Guided Brain Tumor Surgery
In our Center for Neuro-Oncological Neurosurgery, we use 5-ALA fluorescence-guided tumor resection to make malignant gliomas visible during surgery. The dye causes particularly aggressive tumor cells to glow red under blue light, enabling exact delineation of the diseased tissue. In combination with our innovative headlamp loupe system, functional brain mapping, and neurophysiological monitoring, we achieve unprecedented precision: tumors can be removed with maximum safety while crucial brain functions are spared. Simultaneously, we gain high-quality tissue for molecular pathological analyses, paving the way for modern therapies like immunotherapies or personalized vaccines. Thus, we combine the highest surgical safety with the best prerequisites for an individually tailored follow-up treatment.
Brain Tumor Surgery Without an Awake Phase
Brain tumor surgery can also be performed under continuous general anesthesia if particularly valuable functions do not need to be checked via awake surgery. Especially for tumors near areas responsible for movement or sensation, we use state-of-the-art neurophysiological monitoring procedures to minimize risks and preserve important functions.
These procedures include motor evoked potentials (MEPs), which monitor motor pathways. Here, electrical impulses are delivered via electrodes, and their response is measured in the muscles. A drop in signal strength warns us of a possible impairment of motor areas. Additionally, somatosensory evoked potentials (SSEPs) check the pathways for sensory perception: electrical stimuli on arms or legs generate signals that are measured and continuously monitored in the brain. Changes indicate a threat to sensory regions. Furthermore, direct cortical or subcortical stimulation is used. Here, the tissue around the tumor is targetedly electrically stimulated to precisely locate and spare important motor areas.
In combination, these methods act like a real-time monitoring system for the brain: MEPs and SSEPs ensure continuous control of the nerve pathways, while direct stimulation identifies local motor centers. This allows the tumor to be removed as completely as possible without impairing central neurological functions.
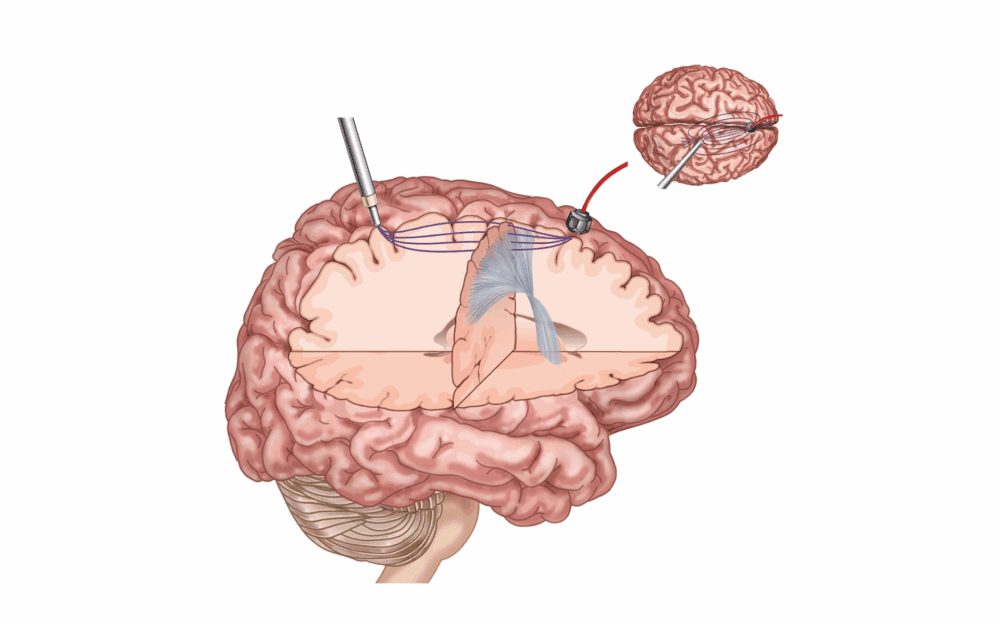
Alternative: Laser Interstitial Thermal Therapy (LITT)
At Beta Klinik, minimally invasive laser interstitial thermal therapy (LITT) is one of the innovative procedures offered by only a few clinics in Europe. Via a thin catheter, laser energy is delivered directly into the tumor tissue under MRI control, heating and destroying it targetedly. The procedure requires only a small skin incision, significantly reducing the risk of infection and speeding up recovery. Especially for deeply located or hard-to-reach tumors, e.g., in the thalamus, the method opens new therapeutic possibilities. However, it is not suitable for all tumor types or sizes.
Which treatment represents the best option in an individual case is decided by the experts from neurosurgery, radiation oncology, neurology, and neuroradiology in the interdisciplinary tumor board. The basis includes imaging, tumor type, general health status, and the patient’s personal therapy goals. While superficially located tumors are often removed microsurgically, LITT can be a gentle alternative for smaller, deeper-seated tumors. In many cases, both procedures can also be combined, for example, if residual tumor tissue remaining after partial removal is treated with laser thermal therapy. Increasingly, LITT is also combined with modern immunotherapeutic approaches to further improve treatment outcomes for brain tumors like gliomas or brain metastases.
Valuable Combination with Immunotherapy
Immunotherapies like checkpoint inhibitors activate the body’s own defenses but face limits with brain tumors: the blood-brain barrier and the immunosuppressive tumor microenvironment hinder their effect.
Laser interstitial thermal therapy (LITT) can support here. The heat exposure destroys tumor cells and releases antigens that stimulate an immune response – similar to a “vaccine effect.” Furthermore, LITT temporarily opens the blood-brain barrier, allowing immunotherapeutic drugs to become more effective. Initial studies indicate that the combination improves tumor control and response to treatment.
At Beta Klinik, we use this approach primarily for gliomas like recurrent glioblastoma and for brain metastases, e.g., from melanomas or lung carcinomas. The combination is particularly suitable when surgery would be risky or if an immunotherapy is already showing effect. After interdisciplinary assessment, LITT may be performed first, followed by an individually adapted immunotherapy with close MRI and laboratory monitoring.
Thus, the combination opens new chances for personalized treatment, especially for aggressive or recurrent brain tumors. We are happy to advise you whether this procedure makes sense in your case. We inform you transparently about all options and support you in the decision. Your well-being and the preservation of your quality of life are the focus.
Different Tumor Types – Individual Surgical Concepts

We Accompany You and Your Life After Brain Tumor Surgery
A successful brain tumor operation is only the first step. At Beta Klinik Bonn, care does not end in the operating room: our interdisciplinary team supports you afterwards as well – with targeted rehabilitation, speech therapy, neurocognitive training, and psychooncological support. Because it’s not just about healing, but about actively and self-determinedly continuing your life.
Your Advantages with Awake Surgery – Safety Through Precision
Awake surgery might seem unusual at first glance – but it is a procedure proven over many years to targetedly protect the brain during brain tumor surgery. Prof. Dr. med. Michael Sabel and Prof. Dr. med. Marion Rapp are among the most experienced surgeons in this field and accompany you empathetically through all phases of the procedure.
Would you like to have it checked whether brain tumor surgery is sensible and safely possible in your case? Simply use our digital pathway:
- Fill out the form: Confirm the data protection declaration and cost coverage.
- Upload findings: e.g., MRI/CT images, surgery reports, doctor’s letters, and/or self-assessment forms.
- Receive surgical assessment: Our specialists evaluate your case and provide a well-founded recommendation.
- The consultation is often useful as an online meeting in the first step, also to clarify initial open questions. If we recommend diagnostics and therapy, you will quickly receive an in-person appointment.
Awake surgery is one of the safest procedures in modern neurosurgery when it comes to protecting important brain functions like speech or movement. For patients, this means: more control, more safety – and often a faster recovery.
These advantages does awake surgery offer:
Healthy brain areas remain protected – we only remove what we can safely justify.
Functions like speech or movement can be tested in real-time during surgery.
Targeted resection spares surrounding tissue – this facilitates rehabilitation.
If speech, memory, or motor skills are preserved, you benefit sustainably in everyday life.
Frequent Questions and Concerns About Surgery
No. The brain has no pain receptors. Thanks to local anesthesia and sedation, you typically only feel a slight pressure sensation. Should pain occur contrary to expectations, it can be quickly and reliably relieved at any time.
You are not alone. We actively accompany you through the surgery. Should overwhelm occur, we can put you back under general anesthesia at any time.
Survival chances after brain tumor surgery depend on many factors: tumor type, location, general health status, and therapy combination.
With slow-growing (low-grade) gliomas, decades of good quality of life can be gained. We now also see patients with practically normal life expectancy, despite the diagnosis of a low-grade glioma. And even with fast-growing gliomas, we now see more and more patients who can gain many years of good quality of life as “long-term survivors.”
All these patients have (often despite unfavorable genetics) one thing in common: They have taken up the fight and carried out and endured the possible therapies.
As with any procedure, brain tumor surgery can involve complications like bleeding, infections, or temporary losses of speech or movement. At Beta Klinik, our experienced neurosurgeons use the most modern procedures to keep such risks as low as possible.
A brain tumor is considered inoperable if it is located such that removal would pose too great a risk to important functions like speech or movement. Even in such cases, we at Beta Klinik individually check alternative treatment paths like radiation therapy, immunotherapy, or study access. Often we find solutions, even if you were told nothing more can be done. It always depends on the individual case