By carrying out an electrophysiological examination, we can detect functional disorders of the nervous system. Normally, we measure the electrical signal processing of nerve and muscle cells during an electrophysiological examination and compare the results with results of healthy patients. We differentiate between nerve cells mainly receiving signals and passing them on (sensory nerve cells) and those that help coordinate an action like the contraction of a muscle (motor nerve cells). Electrophysiological examinations make it possible to investigate if the signal processing of sensory nerve cells (e.g., touching the skin) or motor nerve cells (e.g., contracting a muscle) is disturbed. Generally, the electrical signaling is measured on head, nerves or muscles.
Electrophysiology neurology and epileptology
The carpal tunnel syndrome, for instance, can slow down the nerve conduction velocity due to a pressure damage of a nerve innervating the hand. But also pathological changes due to tumors or inflammations of the hearing nerve, for example, can be tracked with electrophysiological procedures.
Beta Klinik employs the most important neurological-electrophysiological examination procedures, which makes comprehensive diagnostics possible:
- EEG diagnostics
- nerve conduction velocity (NCV)
- electromyography (EMG)
- evoked potentials
- auditory evoked potentials (AEP)
- visually evoked potentials (VEP)
- somatosensory evoked potentials (SSEP)
- electrophysiological examination during surgery
- accompanying internist diagnostics (ECG, long-term ECG, exercise ECG, ultrasound examination)
Auditory evoked potentials
Over a headphone, patients hear several sounds rapidly following each other, generating electric potentials within the acoustic nerve. Electrodes on the surface of the head help measure the electrical potentials, which makes the examination of the acoustic nerve and communicating brain areas of the lower and middle brainstem possible. AEP are regularly measured in case of a suspicion of tumors of the acoustic nerve (e.g., acoustic neuroma), multiple sclerosis or other diseases.
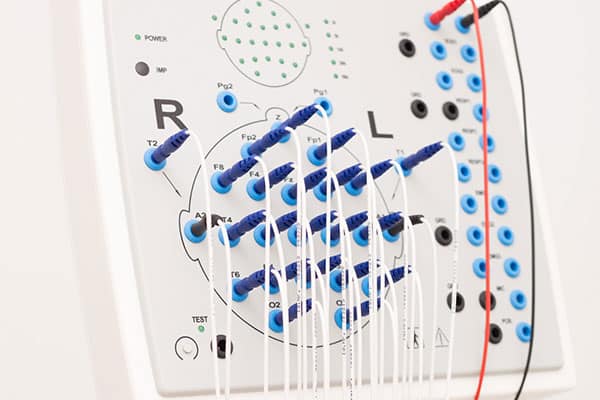
EEG (electroencephalography)
Routine EEG, long-term EEG, sleep deprivation EEG, inpatient video EEG monitoring
Electroencephalography can directly show the tendency of the brain to suffer an epileptic discharges. During EEG, a nurse or a doctor attaches electrodes to the patient´s scalp, which receive electrical impulses from the cerebral cortex. If epilepsy is suspected, a routine EEG provokes epilepsy by hyperventilation and flickering lights.
Within the scope of first diagnostics, EEG serves to localize the focal region in the brain that causes epilepsy in case of focal seizures. Specific questions also may require long-term EEG (e.g., 24 hours), EEG during sleep deprivation or EEG with simultaneous video recording.
An early EEG after an epileptic seizure enables the neurologist to see changes in the wavelengths of the brain, localized slow-downs or waves typical for a certain kind of epilepsy.
Electromyography (EMG)
During electromyography examinations, a needle is inserted into a muscle. The electrical potential generated by the muscle is then measured during different conditions (at rest, slight contraction, maximum contraction). Electromyography makes nuanced diagnoses about muscular diseases (so-called myopathy) possible. Because the production of an electric potential with a muscle depends on the nerve supply, we can also examine disorders of nerves and nerve roots by carrying out electromyography examinations.
Electrophysiological examinations during surgery
The aforementioned electrophysiological examination procedures are also carried out during neurosurgery. This is called intraoperative monitoring (IOM) and provably helps reduce surgical risks (e.g., during removal of tumors in bone marrow or the cerebellopontine angle).
Nerve conduction velocity (NCV)
During the measurement of nerve conduction velocity, motor and sensor nerve cells in arms and legs are excited by electricity. For measuring sensor nerve conduction velocity, electric impulses are generated at the arm, passed on and measured at another location. Measurement of nerve conduction velocity enables us to diagnose pressure damage of nerves or even polyneuropathy (disorder affecting several nerves).
Somatosensory evoked potentials (SSEP)
Applying electric impulses on arms and legs generates somatosensory evoked potentials, which are lead from nerves and bone marrow to the brain. They are recorded by electrodes on the surface of the head. SSEP examinations enable us to investigate the condition of nerves, bone marrow and brain.
Visually evoked potentials (VEP)
A monitor generates visually evoked potentials within the visual nerve and the visual cortex of the brain, by applying stimuli like a changing checkerboard. Electrodes on the surface of the head measure the brainwaves, amplify them and help analyze them. VEP are regularly measured to diagnose functional disorders of the visual system like an inflammation of the visual nerve.