At the Center for Neuro-Oncological Neurosurgery at Beta Klinik Bonn, one central insight is our focus: every therapy begins with thoughtful, high-precision diagnostics. Our goal is not merely to collect imaging data – we analyze, interpret, and relate your findings to your medical history, your life reality, and the most modern therapy options. We consciously leave behind the rigid boundaries of guideline medicine and develop diagnostic pathways that bring genuine added value – especially for tumor recurrences of metastases or gliomas, glioblastomas, or unclear findings after standard treatments.
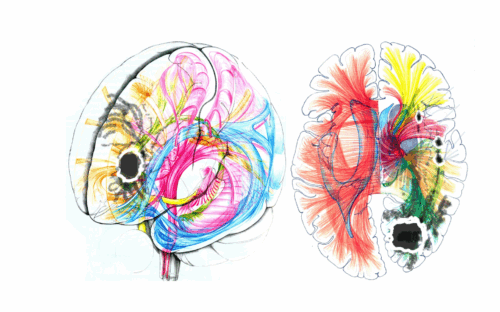
Our team uses state-of-the-art procedures like functional MRI (fMRI), perfusion MRI, spectroscopy, and FET-PET in cooperation, coordinates the diagnostics comprehensively, and derives concrete therapeutic recommendations from them – be it surgery, innovative medicinal immunotherapy, or other alternative non-operative methods.
At our brain tumor center, you benefit from:
- exact differentiation between treatment-related changes and true tumor growth,
- individualized indication for further diagnostics (even in unclear cases),
- years of experience with complex disease progressions,
- a team that always addresses your individual situation.
Differentiating between treatment-related changes like scar tissue and a true tumor recurrence is crucial for the correct treatment. The Center for Neuro-Oncological Neurosurgery at Beta Klinik Bonn uses state-of-the-art procedures for this: high-resolution contrast-enhanced MRI (cMRI), MR perfusion, spectroscopy, and FET-PET in cooperation. These methods provide precise information, forming the basis for individual therapy recommendations and optimal treatment plans.
Contrast-Enhanced MRI (cMRI): Structural Imaging
Contrast-enhanced MRI depicts the tumor’s location, size, and extent in detail. A well-tolerated contrast agent (Gadolinium) is administered intravenously, making leaky blood vessels in the tumor tissue visible. This allows tumors to be clearly distinguished from healthy tissue, especially before treatment. However, scar tissue can also show contrast after surgery or radiation, which is why additional procedures are often used.
MR Perfusion (MRP): Blood Flow Analysis
MR perfusion measures the blood flow in the brain tissue, enabling differentiation between tumor and scar tissue. Tumor tissue is usually more perfused, reflected in increased blood flow volume and vessel density. MRP is particularly valuable for therapy planning and the early detection of recurrences.
Spectroscopy: Chemical Tissue Analysis
Spectroscopy examines the composition of the tissue. Metabolic products like choline, NAA, or lactate are measured. An elevated choline value indicates tumor growth, a decreased NAA value indicates nerve cell damage. As this procedure involves no radiation exposure, it provides additional information about the tumor’s aggressiveness gently. The process is similar to a classic MRI but takes about 10 to 15 minutes longer.
FET-PET: Visualizing Metabolic Activity
FET-PET makes the metabolic activity of tumor cells visible. A weakly radioactive tracer (fluoroethyltyrosine) is administered, which accumulates in the active tumor areas. The procedure has high accuracy in distinguishing recurrence from scar tissue and is particularly useful after surgery or radiation.
Imaging alone is not always sufficient. If the tumor type is not yet clearly identified, a biopsy of the brain tumor may be necessary – either stereotactically (minimally invasive, targeted) or open as part of a planned surgical procedure. The extracted tissue sample is subsequently analyzed neuropathologically and molecular genetically.
Using a biopsy for brain tumor diagnosis, we obtain:
- a confirmed diagnosis (e.g., high-grade vs. low-grade glioma)
- molecular markers for targeted therapies
- information for planning an individualized therapy
Even during the course of the disease – for example, if a tumor recurrence is suspected – a biopsy can help differentiate between active tumor growth and treatment-related changes. For this, we work closely with renowned neuropathologists.
At the Center for Neuro-Oncological Neurosurgery at Beta Klinik Bonn, we also perform open biopsies when imaging alone does not allow a clear statement about the tumor type or when molecular markers are required for selecting targeted therapies. While in a classic (usually stereotactic) biopsy a tiny tissue sample is taken through a very small opening in the skull (burr hole), the open biopsy is performed through a larger cranial opening. The skull is opened specifically to take a larger and more targeted sample from the tumor under direct vision. This offers decisive advantages for diagnostics and subsequent therapy planning.
Our experienced neurosurgeons work with the highest precision to perform the tissue sampling in a function-preserving and low-risk manner. Thanks to state-of-the-art technology like fluorescence-guided tumor visualization, we can make tumor tissue visible during open biopsy or surgery – more precisely, safely, and gently than with conventional methods. We use 5-ALA for gliomas and fluorescein for brain metastases to identify even the smallest tumor parts targetedly and spare healthy tissue (REVEAL™ Fluorescence Guided Surgery).
Our claim: We do not perform biopsies “for their own sake” – we gain diagnostic clarity through them, based on which we can initiate the best possible therapy together.